Music Therapy in the Hospital Setting (Part 2)
During my music therapy internship, our directors encouraged us to write a highlight from the week to share with our team members. I found that most of my patient highlights came from interactions in the hospital setting. There is something so powerful about meeting people in, as one of my directors would remind us, “one of the most difficult moments of their lives.” I found that our biggest role in the hospital setting was giving patients a moment where they were not defined by their diagnosis.
The medical environment can be dehumanizing as it focuses on the patient, not the person. As music therapists, we can provide a safe space where they are allowed to be human; to freely express themselves, and to gain a sense of autonomy in a sterile, restrictive environment.
Below are a few of my “wow” moments from my client interactions in the hospital. I hope they convey a little bit of the magic that can be found in the medical setting.
Music Therapy Moments in the Hospital
Just Keep Singing, 13 September 2021
Three Registered Nurses (RNs) were present when I checked in with the patient. This made me nervous, as I wasn’t sure how the medical staff would respond to having music in the room. I addressed the patient’s attending RN first, and as I introduced myself and the services I could offer, the patient began making noises. The RN closest to her explained that music therapy was in the room. From here I addressed the patient directly, asking if she would like me to play some music for her. She agreed.
The RN closest to her became excited and reminded the patient that because she was currently receiving supplemental oxygen treatment, she might be able to sing with me and have her voice heard. I began to play a standard tune and quickly, the patient began singing along with me. I decided to present some choice-making opportunities for the patient, asking her preference between two songs. She was able to respond with nods and headshakes. Sometimes she grunted “yes” or “no”. We continued singing until she began coughing up fluid from her lungs. The nurses calmed her down as I slowed the tempo and lowered the volume of the music. However, the patient just wanted to keep singing. Between coughs, you could hear her “oo”ing and “ah”ing to the tune of the melody.
I stayed with the patient for the remainder of the oxygen treatment, and for a while after the RNs had left the room. Even after the treatment had stopped and she could no longer hear her own voice, the patient mouthed along with me during each song and at the very end of the session, when I asked her if she would like us to come back to visit her, she turned her head to look at me, taking the time she needed to say “I would love that.”
Lessons Learned:
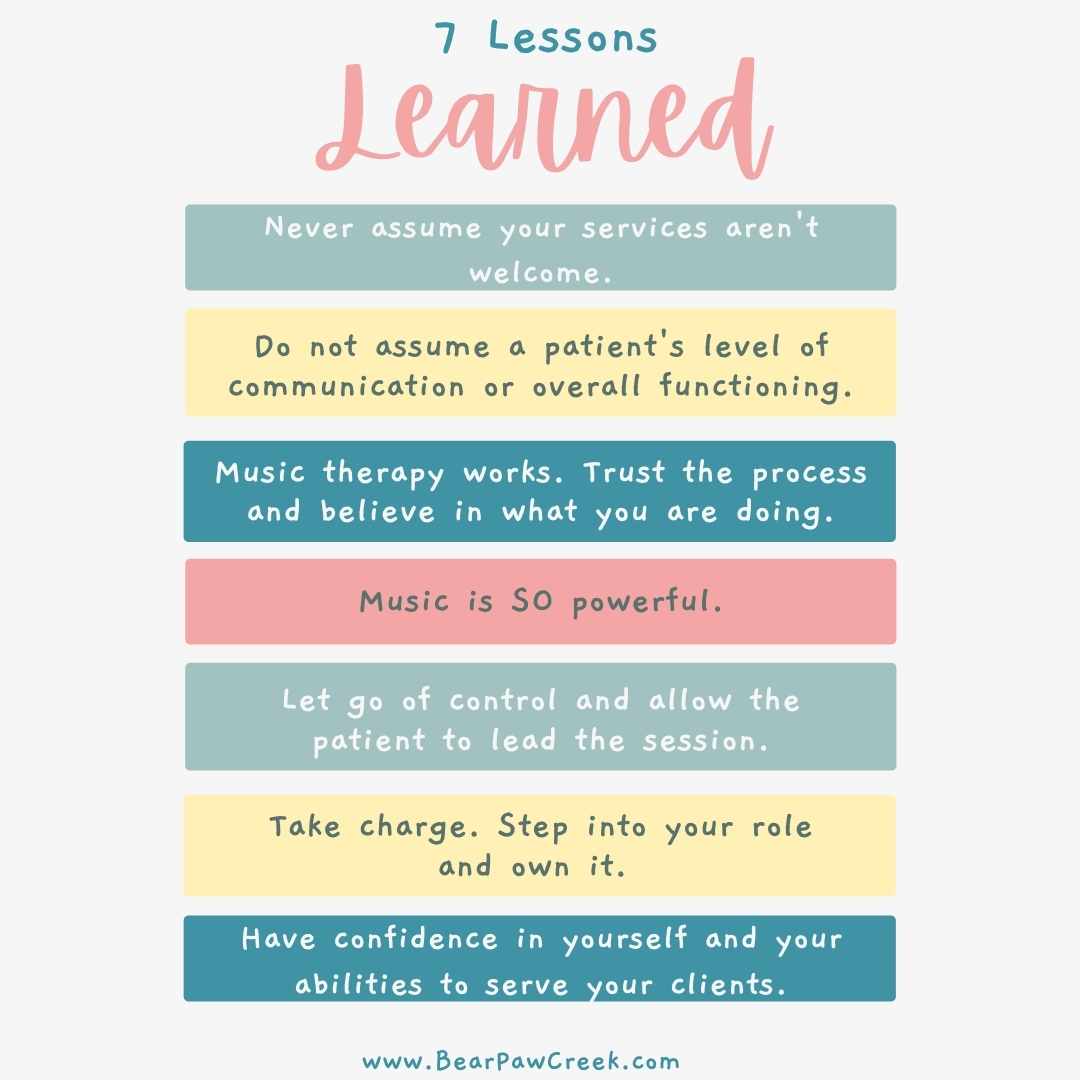
- Never assume your services aren’t welcome. Always give people (patients, doctors, nurses, and other medical staff) the opportunity to accept what you have to offer. It is unfair to assume that your skills are not wanted or needed without asking.
- Do not assume a patient’s level of communication or overall functioning. Provide them with opportunities to show you how they are feeling and what they are capable of.
- Music therapy works. This patient increased her ability to handle the oxygen treatment from 3 minutes to 15 minutes because the music was so motivating for her. Trust the process and believe in what you are doing.
Part 2 of Music Therapy in the Hospital Setting by Whitney Perry. Click Here to Read About Music Therapy Moments in the Hospital. Share on X
The Power of Music
Vibin’, 22 November 2021
While some patient interactions require a certain level of emotional intensity, sessions that are positive, lighthearted, or easygoing can be just as impactful. It is okay to have fun with your clients. Just remember to be flexible and follow their lead.
My supervisor and I arrived at the room of a patient we had seen together once before. As we entered and introduced ourselves, the patient frustratedly exclaimed “I’ve been asking for you all week, what took you so long?!” He expressed no interest in music, stating that he was in too much pain. As he began eating his food we asked if we could play something relaxing for him as a distraction, and he agreed saying “a little dinner music would be nice.” I began to play “Ain’t No Sunshine” at a low volume and slow tempo, and soon enough he was conducting and playing along with his silverware.
We upped the tempo and emphasized the beat, playing through the song continuously for about 6 minutes. From here we moved into “Down on the Corner,” jamming for 12 minutes. My supervisor placed a drum next to the patient, and soon he was controlling the tempo and rhythm for us for 40 minutes of straight music, no pauses at all. He was in a trance-like state, eyes closed, body relaxed, providing the grounding for all three of us. Anytime we slowed the music down to come to a close, he would open his eyes, smile, and continue playing. As we finally brought the session to a close, he stated he was feeling so much better than “20 minutes–oh–an hour ago” and asked that we “go make someone else feel as good as I do.”
Lessons Learned:
- Music is SO powerful. We talked with this patient about the inherent rhythm in all of us in so many different things we do. It was incredible to see how music transformed his state in such a short time, though he originally seemed uninterested in services.
- Let go of control and allow the patient to lead the session.
Focus on Me, 27 September 2021
Some sessions you will never forget, simply because of the impact they have on you.
When I arrived at this patient’s room, I noticed that she was on contact precautions. The patient’s attending nurse was in the room, and I consulted with her to see if she could ask the patient if she would like music therapy services. The patient said yes.
As I finished putting on my gown and gloves I heard the patient begin to choke. Her breathing became intensely labored and her nurse called for help. Another nurse rushed into the room and the two of them held her down on the bed and forcefully told her to begin taking deep breaths. The patient’s breathing became more and more labored as I entered the room. I started to play the guitar in time with the nurses instructions in an attempt to help create a stable pattern for the patient to follow. After about a minute of playing in the background with no change in the patient’s condition, I asked the nurses if it would be okay for me to try something.
They agreed and I positioned myself directly in front of the patient, instructing her to focus on me, the sound of the music and the sound of my voice. I guided the patient through some deep breaths, prompting her to breathe in and out in time with the chord changes I played. Immediately the patient began to calm down. One of the nurses audibly said “wow”. As the patient continued to relax and her breathing came back down to normal, I began to hum “Blowin in the Wind”. She maintained eye contact with me as I hummed before eventually closing her eyes. I began to sing the lyrics of the song, and when I reached the chorus, she joined in singing with me: “the answer my friend, is blowing in the wind. The answer is blowing in the wind”.
Our session continued with the patient requesting more and more songs to sing together. She disclosed a lot of her medical, musical and personal history without any prompting at all, and asked that I come back to visit her on Thursday.
Lessons Learned:
- Take charge. Step into your role and own it.
- Have confidence in yourself and your abilities to serve your clients. This confidence will empower you and be a blessing to your patients as well.

